Funeral Directing
Are You Suffering from Compassion Fatigue?
If you think you are suffering from Compassion Fatigue, Burnout or Secondary Trama, THIS TEST IS VERY IMPORTANT! If you’re like me, you may think you’re suffering, but you won’t reach out for help until you have an objective voice confirming your own perceptions. This test is that secondary voice! If you “fail”, it’s time for you to consider seeking professional care!
There’s a difference between burnout and compassion fatigue. Burnout in the workplace is a more general term that relates to anybody in a stressful situation, while compassion fatigue is a phenomena that specifically relates to those of us who are professional caregivers.
Being that funeral directors are susceptible to compassion fatigue AND have an uncontrolled work environment, we are especially vulnerable to burnout, as well as secondary trama. I’ve bordered compassion fatigue and burnout a couple times as an undertaker, and sometimes I’ve crossed the line into the danger zone where dark depression and self-infliction reside.
And I’ve often wondered if there’s a way to define whether or not a caregiver (such as a funeral director, nurse, doctor, etc.) is indeed suffering from compassion fatigue and/or burnout.
Here’s a test I found.
It’s long. And if you want to complete it, it might take about 15 minutes. Probably the easiest way to take it is to print out this entire article by using the “Print” button at the bottom. If you “fail” the test, seek help.
When you [help] people you have direct contact with their lives. As you may have found, your compassion for those you [help] can affect you in positive and negative ways. Below are some questions about your experiences, both positive and negative, as a [helper]. Consider each of the following questions about you and your current work situation.
Select the number that honestly reflects how frequently you experienced these things in the last 30 days.
1=Never 2=Rarely 3=Sometimes 4=Often 5=Very Often
1. I am happy.
2. I am preoccupied with more than one person I [help].
3. I get satisfaction from being able to [help] people.
4. I feel connected to others.
5. I jump or am startled by unexpected sounds.
6. I feel invigorated after working with those I [help].
7. I find it difficult to separate my personal life from my life as a [helper].
8. I am not as productive at work because I am losing sleep over traumatic experiences of a person I [help].
9. I think that I might have been affected by the traumatic stress of those I [help].
10. I feel trapped by my job as a [helper].
11. Because of my [helping], I have felt “on edge” about various things.
12. I like my work as a [helper].
13. I feel depressed because of the traumatic experiences of the people I [help].
14. I feel as though I am experiencing the trauma of someone I have [helped].
15. I have beliefs that sustain me.
16. I am pleased with how I am able to keep up with [helping] techniques and protocols.
17. I am the person I always wanted to be.
18. My work makes me feel satisfied.
19. I feel worn out because of my work as a [helper].
20. I have happy thoughts and feelings about those I [help] and how I could help them.
21. I feel overwhelmed because my case [work] load seems endless.
22. I believe I can make a difference through my work.
23. I avoid certain activities or situations because they remind me of frightening experiences of the people I [help].
24. I am proud of what I can do to [help].
25. As a result of my [helping], I have intrusive, frightening thoughts.
26. I feel “bogged down” by the system.
27. I have thoughts that I am a “success” as a [helper].
28. I can’t recall important parts of my work with trauma victims.
29. I am a very caring person.
30. I am happy that I chose to do this work.
SCREENING
Based on your responses, place your personal scores below. If you have any concerns, you should discuss them with a physical or mental health care professional.
COMPASSION SATISFACTION
Compassion satisfaction is about the pleasure you derive from being able to do your work well. For example, you may feel like it is a pleasure to help others through your work. You may feel positively about your
colleagues or your ability to contribute to the work setting or even the greater good of society. Higher scores
on this scale represent a greater satisfaction related to your ability to be an effective caregiver in your job.
Test Results Scale for Compassion Satisfaction
3. ____ 6. ___ 12. ____ 16. ____ 18. ____ 20. ____ 22. ____ 24. ____ 27. ____ 30. ____ Total: _____
The sum of my Compassion Satisfaction questions:
22 or less 43 or less = Low // Between 23 and 41 = Average // 42 or more = High
BURNOUT
Most people have an intuitive idea of what burnout is. From the research perspective, burnout is one of the elements of Compassion Fatigue (CF). It is associated with feelings of hopelessness and difficulties in dealing
with work or in doing your job effectively. These negative feelings usually have a gradual onset. They can
reflect the feeling that your efforts make no difference, or they can be associated with a very high workload or
a non-supportive work environment. Higher scores on this scale mean that you are at higher risk for burnout.
Test Results Scale for Burnout:
*1. ____ *4. ____ 8. ____ 10. ____ *15. ____ *17. ____ 19. ____ 21. ____ 26. ____ *29. ____
Total: ____
22 or less = Low // Between 23 and 41 = Average // 42 or more = High
SECONDARY TRAUMA
The second component of Compassion Fatigue (CF) is secondary traumatic stress (STS). It is about your work related, secondary exposure to extremely or traumatically stressful events. Developing problems due to exposure to other’s trauma is somewhat rare but does happen to many people who care for those who have experienced extremely or traumatically stressful events. For example, you may repeatedly hear stories about the traumatic things that happen to other people, commonly called Vicarious Traumatization. If your work puts you directly in the path of danger, for example, field work in a war or area of civil violence, this is not secondary exposure; your exposure is primary. However, if you are exposed to others’ traumatic events as a result of your work, for example, as a therapist or an emergency worker, this is secondary exposure. The symptoms of STS are usually rapid in onset and associated with a particular event. They may include being afraid, having difficulty sleeping, having images of the upsetting event pop into your mind, or avoiding things that remind you of the event.
Test Results Scale for Secondary Trama
2. ____ 5. ____ 7. ____ 9. ____ 11. ____ 13. ____ 14. ____ 23. ____ 25. ____ 28. ____ Total: _____
22 or less = Low // Between 23 and 41 = Average // 42 or more =High
IF YOU WANT MORE ANALYSIS OF YOUR SCORE, CLICK HERE: PROFESSIONAL QUALITY OF LIFE SCALE (PROQOL) COMPASSION SATISFACTION AND COMPASSION FATIGUE (PROQOL) VERSION 5 (2009)
My Job Proposed and I Said “No”
It’s been 30 straight days since I’ve had a day off.
Work has never hurt me. Good work is fuel to the body and soul. And the funeral business is good work. It is meeting needs that only you – as funeral director – can meet. It’s easing an otherwise impossible task for the bereaved. It’s so good that many directors marry this business. It’s easy to marry this business.
To commit to it as your first love. It’s easy to pledge your heart to this one thing and no other.
It’s easy to let your own family take second in your priority list.
It’s easy to allow your personal life to get swallowed up by the voracious appetite of death care.
Like many other businesses, if you don’t marry it, it begs. It begs for your attention. Your time. It begs for your heart. It begs for your soul. It begs for you to miss your kid’s games. It begs of you to skip the date night with your special someone. It begs you to miss church.
This business will take you and romance you into believing that you … YOU are THE ONE … the only one who can meet the needs of the family.
And I’m afraid that one day I’ll give up and concede. I’ve been in this business for 10 years now and if feels like it’s becoming less and less “what I do” and more and more “who I am.”
And I have nothing against committing to a job for a lifetime; my problem is having my sense of freedom erode day by day. The more I become embedded, the harder it will become to “get out” … if I should ever choose to “get out.” Will I eventually marry this business and sacrifice my dreams to earn a Ph.D.? Will I become like so many others and just let this business take my soul?
It’s not the hard work, the late hours, the fact that I didn’t get done working until 1 AM this morning … it’s the fact that it’s slowly eating away at me. I’m becoming this business and this business is becoming me.
I love caring for families, helping them walk through the valley of the shadow. I enjoy putting my heart into this business, but I won’t give it my soul.
I haven’t married it. I won’t marry it. I won’t let it define me.
And this is why:
Make Your Face into an Urn
If you want the details on how you can turn your face into an urn, you can click here. Otherwise, just enjoy these four slightly creepy but neat personalized urns from Cremation Solutions.
1. This one’s my favorite ….

2. And who wouldn’t want to put their ashes in Barack Obama’s head?

3. I think this one is Elizabeth Hurley.
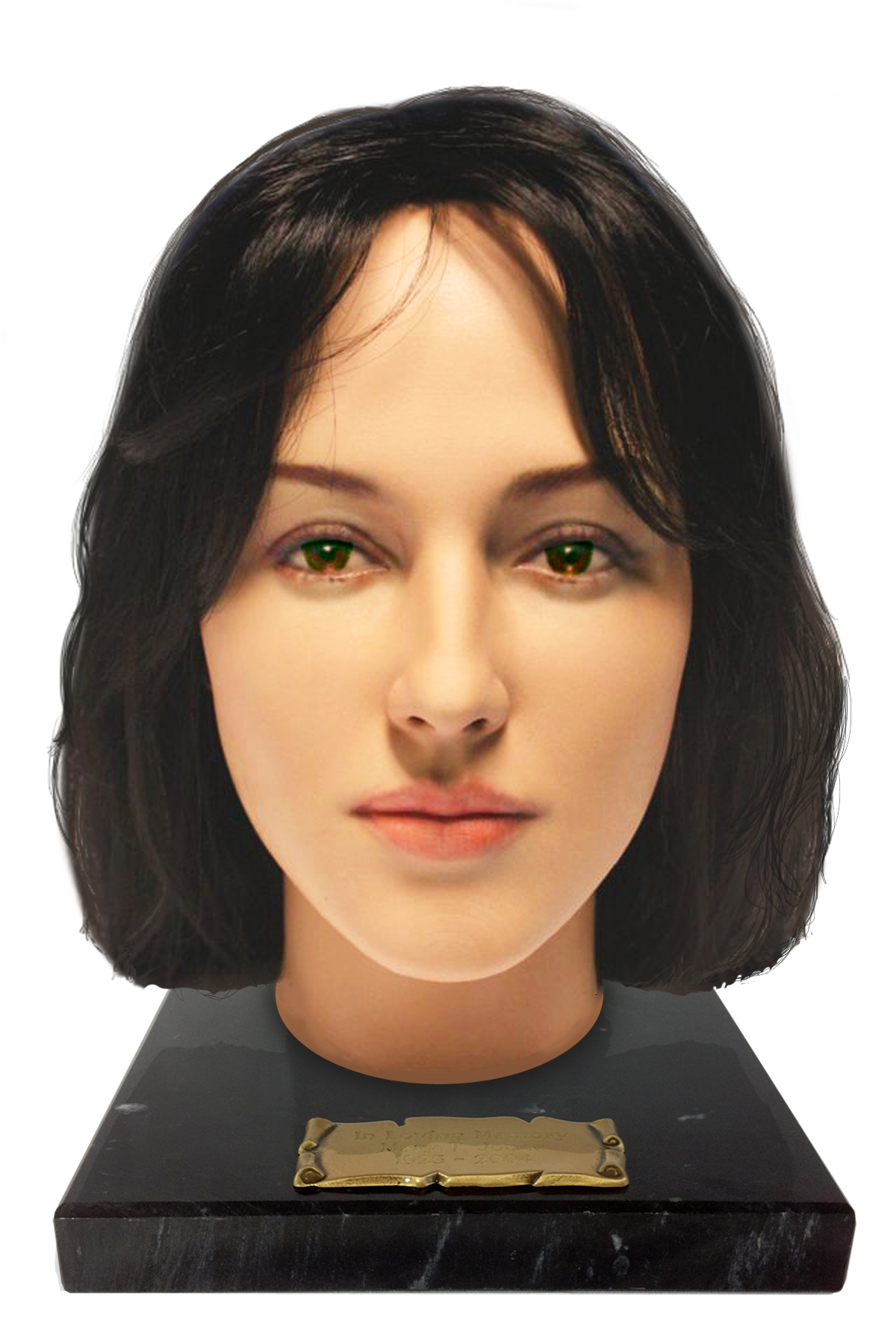
4. Cate Blanchett. Lord of the Rings fans can put themselves in Cate’s head.

Whose head would you want to put your ashes in?
5 Ways to Avoid Burnout
There’s a difference between burnout and compassion fatigue. Burnout in the workplace is a more general term that relates to anybody in a stressful situation, while compassion fatigue is a phenomena that specifically relates to those of us who are professional caregivers.
Being that funeral directors are susceptible to compassion fatigue AND have an uncontrolled work environment, we are especially vulnerable to burnout.
Here are five strategies to avoid burnout as advised by the Handbook of Thanatology:
1. Practice responsible selfishness, recognizing one’s own needs as important as the needs of others. The external demands imposed on the professional helper coupled with the internal belief that one’s own needs are secondary to those of others can significantly drain a person’s emotional energy.
2. Separate work from home. Use the transition time between work and home to “emotionally decompress”, or “shift gears.” Techniques such as mental imagery, e.g., visualizing the pressures of work evaporation; distraction, e.g. listening to music during the drive home; or getting physical exercise, can be helpful.
3. Develop positive support groups, either formal self-help groups or informal empathetic groups.
4. Remember to laugh. Laughter offers tremendous benefit and can provide a powerful antidote to the toxicity of chronic stress.
5. Redefine “success.” For professionals who are passionately dedicated to their work and have a strong desire to be successful, a sense of personal failure is a tremendous source of stress and burnout. (from page 384).
How to Speak the Language of Grief
You walk into a house full of fresh grief. It’s fresh because the death just occurred. Your best friend’s husband went out to the bar last night, drowned his hard day in hard drink and he never made it back home. Fresh. Because both you and your friend have never experienced death this close.
You open the door like you have so many times before, but this time the familiarity of the house is unexpected different, dark and lonely. What once housed parties, life and love now houses something you’ve never known before. Like a river, everything is in the same place it was when you last saw it, but this home has changed.
You see your friend’s children sitting on the sofa, staring into space.
You ask them, “Where’s your mom?”
And as you reach to hug them, they snap back to reality and whisper, “Upstairs.”
Each step brings you closer to what you know is only an apparition of your friend. The nerves build. Fear begins to build. You repress it as you ready yourself to meet your closest friend who has all of a sudden become someone you may no longer know.
“Can I come in?” you ask. No response.
You push open the cracked bedroom door and see the body of your friend collapsed on her bed, with used tissues surrounding her like a moat.
You tip-toe into the room, slowly sit down on the bed, and not sure if she’s awake or asleep, you reach for your friends shoulder and begin rubbing her back. Her blood shot eyes open, look at you and then, they slowly look through you.
You fill the weird silence with an “It’s going to be alright”.
“It’s not”, she whispers. “I’m alone with two kids and no job.” Her voice suddenly raises as anger courses through her body, “Why the f*** would he do this to me?”
The curse word chides you into recognizing that you’ve not only misspoken, but you’ve spoken too soon, so you decide to wait in silence. She starts to cry. You respond to her tears with your own. Even though you want to respond with words, you know this isn’t the time for words. There’s no perfection words here. There’s no perfect anything here. And so you wait.
You stay. Listen. Silence. You take her pain into your soul. Hours pass. She rises out of bed and makes the children dinner.
You’ve spoken, not with words or advice; not by trying to solve the problem; nor by placing a limit on your time. You’ve taken the uncomfortable silence, allow the grace for tears, for brokenness; you’ve allowed yourself to sit in the unrest without trying to fix it.
With your presence. With your love. In your honest acknowledgement of real loss, you’ve spoken the language of grief.
Although the language of grief is usually spoken in love, presence and time, sometimes it’s spoken in words. And when it is, here are five practical “do”s and “don’ts”
The “DON’T”S:
1. At least she lived a long life, many people die young
2. He is in a better place
3. She brought this on herself
4. There is a reason for everything
5. Aren’t you over him yet, he has been dead for awhile now
The “DO”S:
1. I am so sorry for your loss.
2. I wish I had the right words, just know I care.
3. I don’t know how you feel, but I am here to help in anyway I can.
4. You and your loved one will be in my thoughts and prayers.
5. My favorite memory of your loved one is…